A patient registry has been launched in New Zealand to improve access to the underutilised therapy, which is proven to make the lives of pancreatic cancer patients much more "bearable".
The PERT treatment is known to improve digestion, slow the rate of weight loss, improve quality of life and allow people with pancreatic cancer to better tolerate chemotherapy.
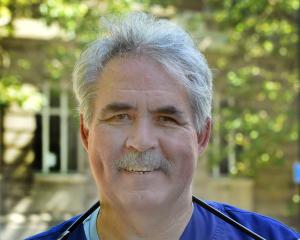
The registry is being hosted by the Aotearoa Australia Pancreatic Enzyme Replacement Therapy research group, led by University of Otago (Christchurch) department of medicine head and palliative care physician Dr Amanda Landers.
In a media release from the University of Otago, she said the mission was to make sure every New Zealand and Australian patient with pancreatic cancer got assessed by a dietitian and was given access to PERT medication, if possible.
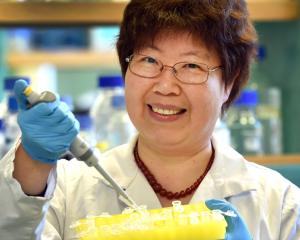
PERT is a biological enzyme medication — better known as creon — which is derived from pig’s liver and administered in pill form.
"This therapy not only makes the last weeks and months of a patient’s life more bearable and less miserable, but can potentially extend survival by helping them to better absorb the nutrients in their food, and to tolerate chemotherapy and other treatments."
Too few of the 700 New Zealand patients diagnosed with pancreatic cancer each year were given access to PERT.
"Its use is variable at best, both here and in Australia, even though it’s standard treatment in other parts of the world.
"That’s due to a lack of awareness from both patients and clinicians."
Results from a recent study published by Dr Landers and her colleagues showed 40% of New Zealand European pancreatic cancer patients and 45% of Māori patients had never heard of PERT treatment.
That was not helped by the fact that only a quarter of New Zealand patients diagnosed with pancreatic cancer even got to see a cancer specialist.
"Once diagnosed, many patients don’t get referred on, due to their poor prognosis."
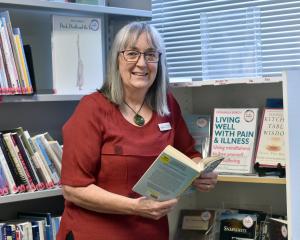
It was hoped the new patient-reported registry and accompanying online survey would help fix the issue.
Pancreatic cancer has a very poor prognosis. It has a five-year survival rate of only 5%.
On average, there are only 92 days between diagnosis and death, because the cancer is diagnosed late, hides itself in the body, and symptoms are hard to identify and isolate.
There is no known cure except for surgery if caught early enough.